Request an Appointment
(703) 719-2040
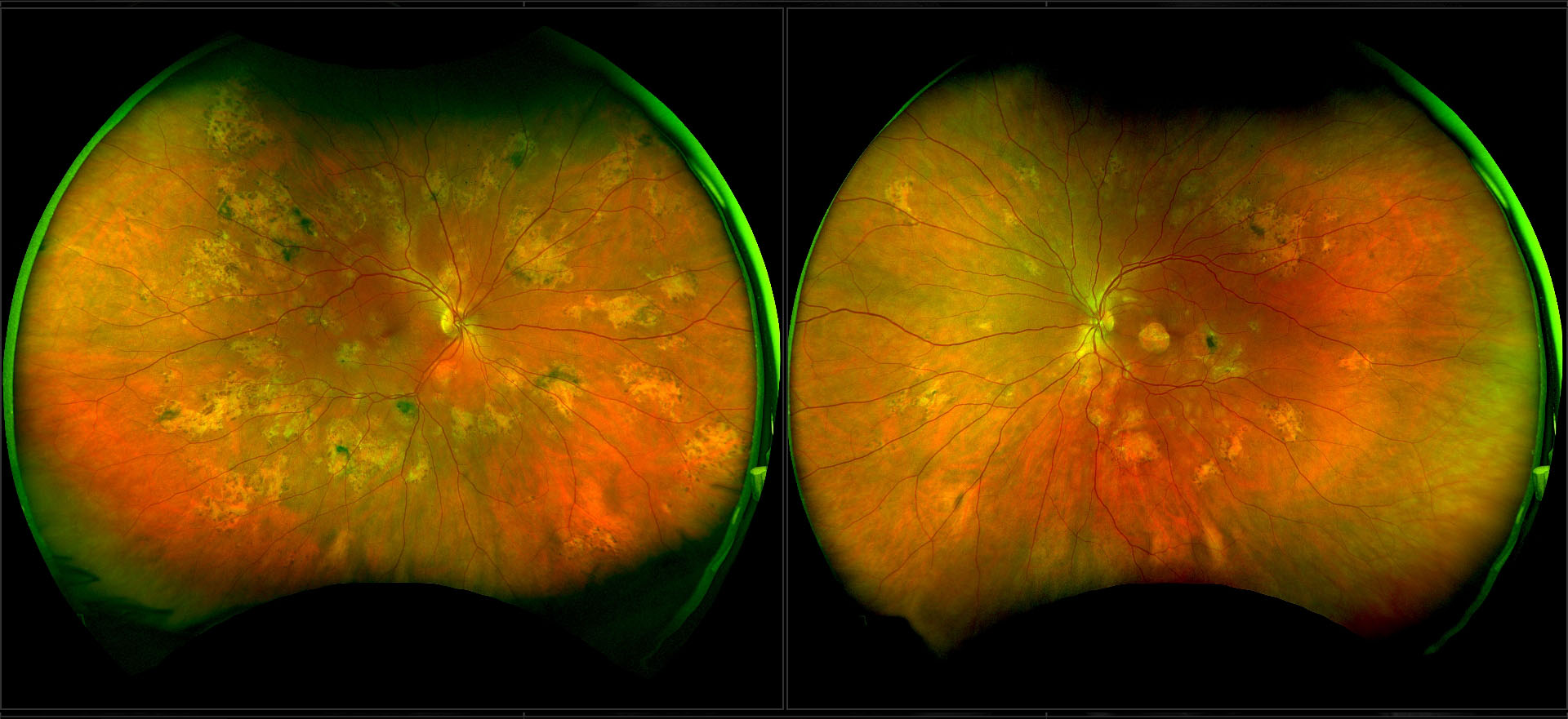
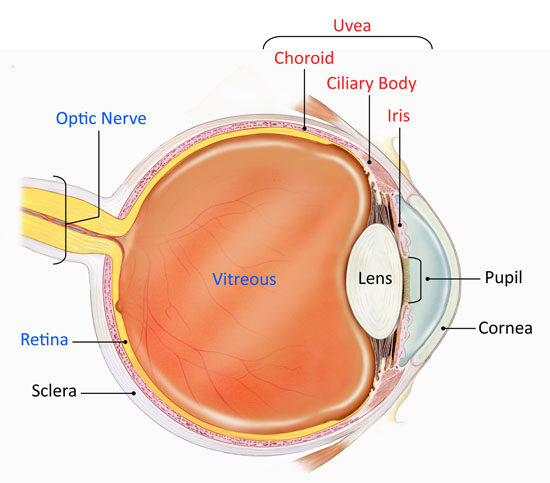
Uveitis occurs when the middle layer of the eyeball gets inflamed. This layer, called the uvea, has many blood vessels that nourish the eye. Uveitis can damage vital eye tissue, leading to permanent vision loss.
The uvea is the middle layer of the eye between the sclera (white part of the eye) and the retina (light-sensitive layer at the back of the eye). It has 3 parts:
Uveitis is not a single disease. Similar to arthritis (joint inflammation), uveitis can be a part of many different disease processes. Different types of uveitis often follow characteristic patterns that are distinguished by factors such as part of the eye that is affected, if the inflammation involves one or both eyes, or if the inflammation began suddenly or gradually.
There are 4 types of uveitis. They are based on which part of the uvea is primarily affected.
The cause may not always be clear. However, causes and risk factors include:
Uveitis can develop suddenly. Symptoms can include:
Evaluation for uveitis includes a detailed, complete eye exam and a thorough review of health history. Since uveitis is often connected with other diseases or conditions, various diagnostic tests may be needed. These may include blood or urine tests, examination of eye fluids, and imaging tests, such as X-rays and MRI scans. If there is a possible underlying condition as the cause of uveitis, referral to another specialist for further evaluation including general medical examination and additional laboratory tests may be necessary.
Uveitis needs to be treated timely to prevent lasting problems. Treatment often includes eye drops that reduce inflammation (corticosteroids, non-steroidal anti-inflammatories) and widen (dilate) the pupil, which also help reduce eye pain and light sensitivity. In some cases, there may be a need for eye injections or additional systemic treatment. In some cases, uveitis specialist will work and co-manage with other specialists including rheumatologists to help treat the condition.
If uveitis is caused by an underlying condition, treatment may focus on that specific condition. Usually, the treatment for uveitis is the same regardless of the associated cause, as long as it is not infectious. The goal of treatment is to resolve the inflammation in the eye, as well as in other parts of the body, if present. In some cases, treatment may last for months to years.
