Request an Appointment
(703) 719-2040
Peripheral diabetic retinopathy, the advanced form of diabetic retinopathy, is characterized by the development of new blood vessels in the retina and its growth into the vitreous. Although these new blood vessels arise in response to circulation problems, they are abnormal and fragile. As a result, bleeding, scarring, and even retinal detachment can ensue. Without treatment, these problems can lead to severe and permanent vision loss.
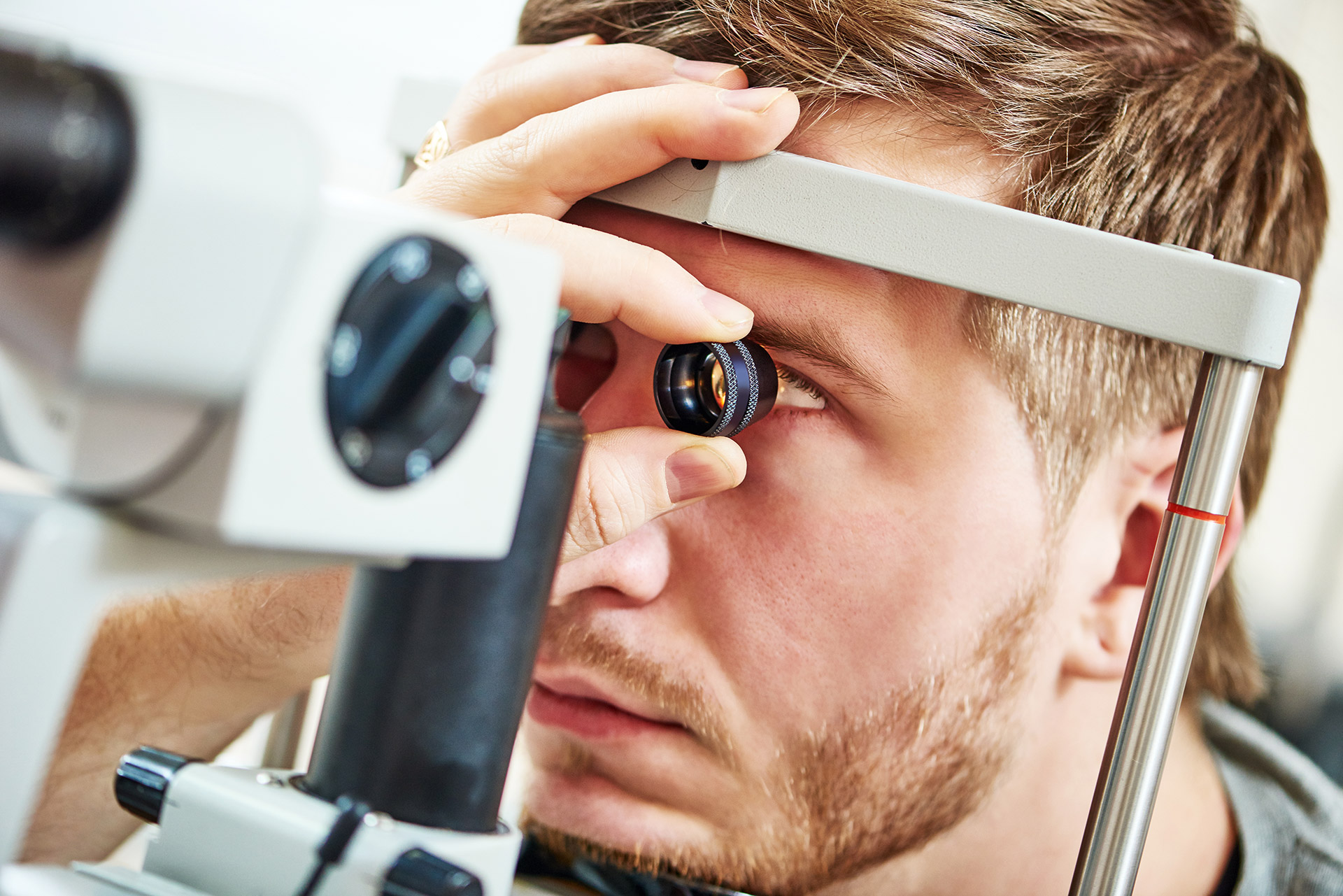
Panretinal photocoagulation (PRP), or scatter photocoagulation, is a laser procedure designed to stop the unhealthy leakage of blood and fluid into the retina. While it does not cure proliferative diabetic neuropathy, it can help stabilize the situation and reduce the risk of further vision loss by decreasing the chances of vitreous hemorrhage and tractional retinal detachment.
Typically performed as an in-office procedure, panretinal laser photocoagulation involves creating minuscule burns at multiple spots in the peripheral retina to shrink the abnormal blood vessels, prevent them from leaking, and inhibit their continued growth. Sometimes multiple treatments are required.
Although panretinal photocoagulation offers demonstrated effectiveness for reducing the risk of severe vision loss in people with high-risk proliferative diabetic retinopathy, there are potential side effects and risks. While it fulfills the goal of protecting and preserving as much central vision as possible, panretinal photocoagulation will cause some peripheral vision loss. It may also result in diminished night vision and limit one's ability to focus up close. Another post-operative consequence is that the procedure can cause blurriness. However, in most cases, this blurriness is temporary and eventually resolves.
Our retinal specialist will also recommend if additional procedures, such as anti-VEGF injections or a surgical procedure, such as vitrectomy, are needed to achieve optimal results.
