Request an Appointment
(703) 719-2040

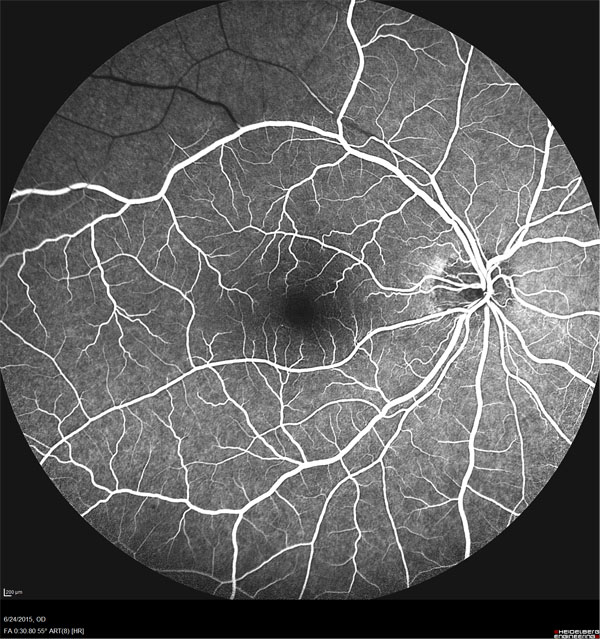
The process of converting reflected light into images begins at the retina, a thin layer of tissue at the back of the eye. Here millions of photoreceptor cells translate the incoming and focused light into full-color visual information that then heads to the brain, where it's instantly interpreted and defined.
When your eyes are healthy, this intricate process operates seamlessly. Just as every part of the body requires a constant and unimpeded blood supply bringing oxygen and nutrients from the heart and carrying deoxygenated blood back to it, so do vital structures within the eye.
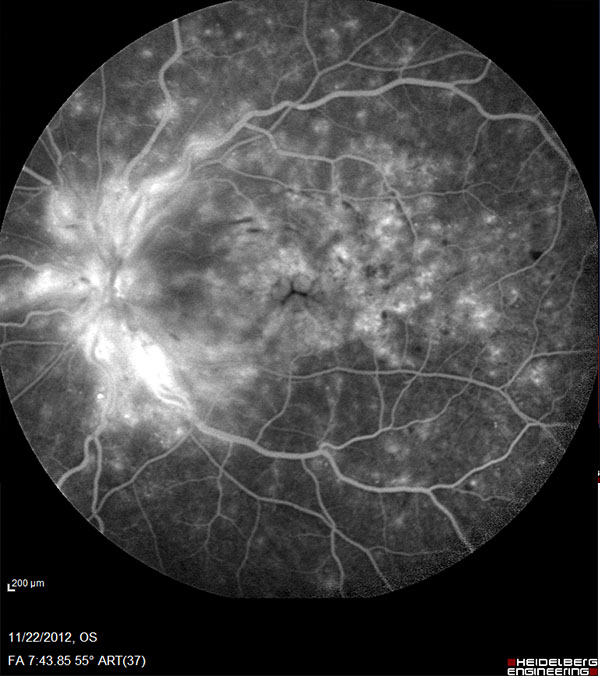
Retinal vein occlusion (RVO) occurs when the blood flow heading back to the heart gets blocked. With no means for the blood to drain, hemorrhages (bleeding) and leakage from the blocked blood vessels can ensue. While RVO can develop due to narrow retinal veins, people with diabetes, high cholesterol, high blood pressure, and other circulation issues have a higher risk.
A branch retinal vein occlusion (BRVO) and a central retinal vein occlusion (CRVO) describe the two main locations where retinal vein occlusion can occur.
Central vein retinal occlusion develops from a blood clot or reduced blood flow in the central retinal vein that drains the retina. Most patients with CRVO develop it in one eye, and its specific cause is still unknown.
The common risks factors for CRVO include:
A branch retinal vein occlusion typically occurs when a branch retinal artery, affected by the hardening of the arteries, compresses a branch retinal vein.

The common risk factors for BRVO include:
It’s essential to be aware of the signs and symptoms of RVO so that you can get prompt, appropriate care. Typically occurring in just one eye, blurring and vision loss may be initially subtle and painless but can quickly worsen.
Mild CRVO may show no symptoms. However:
BRVO causes a sudden, painless loss of vision. If the affected area is not in the center of the eye, BRVO can go unnoticed with no symptoms.
In addition to treating medical conditions that contribute to RVO, you may need specific intravitreal injections, focal laser therapy, or pan-retinal photocoagulation therapy. These methods can help address damaging edema and the development of abnormal blood vessels.
It’s important to note that early detection of macular edema or abnormal blood vessels is important; most patients can avoid severe vision loss if treatment is initiated before substantial damage develops in the eye.
